
What's New

Bioprinting research from the lab of Rice University bioengineer Jordan Miller featured a visually stunning proof-of-principle -- a scale-model of a lung-mimicking air sac with airways and blood vessels that never touch yet still provide oxygen to red blood cells. Credit: Jordan Miller/Rice University
Bioengineers have cleared a major hurdle on the path to 3-D printing replacement organs with a breakthrough technique for bioprinting tissues.
The new innovation allows scientists to create exquisitely entangled vascular networks that mimic the body's natural passageways for blood, air, lymph and other vital fluids.
The research is featured on the cover of this week's issue of Science. It includes a visually stunning proof-of-principle—a hydrogel model of a lung-mimicking air sac in which airways deliver oxygen to surrounding blood vessels. Also reported are experiments to implant bioprinted constructs containing liver cells into mice.
Bioengineers have cleared a major hurdle on the path to 3D printing replacement organs with a breakthrough technique for bioprinting tissues with exquisitely entangled vascular networks that mimic the body's natural passageways for blood, air, lymph and other vital fluids. The research appears in the May 3 issue of Science and includes a hydrogel model of a lung-mimicking air sac in which airways deliver oxygen to surrounding blood vessels. The research team also reported experiments to implant bioprinted constructs containing liver cells into mice. Credit: Brandon Martin/Rice University
The work was led by bioengineers Jordan Miller of Rice University and Kelly Stevens of the University of Washington (UW) and included 15 collaborators from Rice, UW, Duke University, Rowan University and Nervous System, a design firm in Somerville, Massachusetts.
"One of the biggest road blocks to generating functional tissuereplacements has been our inability to print the complex vasculature that can supply nutrients to densely populated tissues," said Miller, assistant professor of bioengineering at Rice's Brown School of Engineering. "Further, our organs actually contain independent vascular networks—like the airways and blood vessels of the lung or the bile ducts and blood vessels in the liver. These interpenetrating networks are physically and biochemically entangled, and the architecture itself is intimately related to tissue function. Ours is the first bioprinting technology that addresses the challenge of multivascularization in a direct and comprehensive way."
Researchers identify biomarker for chronic fatigue syndrome
by Stanford University Medical Center
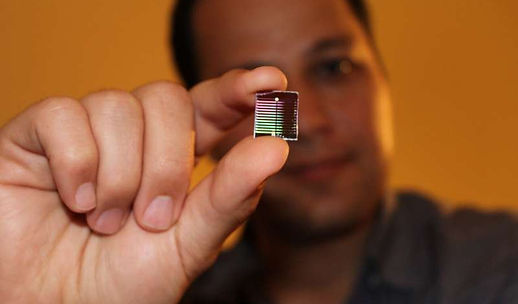
A diagnostic device for ME/CFS. Credit: R. Esfandyarpour
People suffering from a debilitating and often discounted disease known as chronic fatigue syndrome may soon have something they've been seeking for decades: scientific proof of their ailment.
Researchers at the Stanford University School of Medicine have created a blood test that can flag the disease, which currently lacks a standard, reliable diagnostic test.
"Too often, this disease is categorized as imaginary," said Ron Davis, Ph.D., professor of biochemistry and of genetics. When individuals with chronic fatigue syndrome seek help from a doctor, they may undergo a series of tests that check liver, kidney and heart function, as well as blood and immune cell counts, Davis said. "All these different tests would normally guide the doctor toward one illness or another, but for chronic fatigue syndrome patients, the results all come back normal," he said.
The problem, he said, is that they're not looking deep enough. Now, Davis; Rahim Esfandyarpour, Ph.D., a former Stanford research associate; and their colleagues have devised a blood-based test that successfully identified participants in a study with chronic fatigue syndrome. The test, which is still in a pilot phase, is based on how a person's immune cells respond to stress. With blood samples from 40 people—20 with chronic fatigue syndrome and 20 without—the test yielded precise results, accurately flagging all chronic fatigue syndrome patients and none of the healthy individuals.
The diagnostic platform could even help identify possible drugs to treat chronic fatigue syndrome. By exposing the participants' blood samples to drug candidates and rerunning the diagnostic test, the scientists could potentially see whether the drug improved the immune cells' response. Already, the team is using the platform to screen for potential drugs they hope can help people with chronic fatigue syndrome down the line.
A paper describing the research findings will be published online April 29 in the Proceedings of the National Academy of Sciences. Davis is the senior author. Esfandyarpour, who is now on the faculty of the University of California-Irvine, is the lead author.
Providing the proof
The diagnosis of chronic fatigue syndrome, when it actually is diagnosed, is based on symptoms—exhaustion, sensitivity to light and unexplained pain, among other things—and it comes only after other disease possibilities have been eliminated. It's estimated that 2 million people in the United States have chronic fatigue syndrome, but that's a rough guess, Davis said, and it's likely much higher.
